Integrating Wearables and Remote Patient Monitoring Data into Clinical Workflows
Health systems are moving beyond pilots with remote patient monitoring (RPM) and wearables. The focus is shifting from collecting raw sensor data to embedding clinically reliable information into everyday workflows. That means standardized data, clear governance, and seamless EHR integration.
The stakes are high. U.S. claims for RPM services grew by more than 1,300% between 2019 and 2022 (Definitive Healthcare), showing that adoption is no longer experimental. Yet many organizations struggle with alert fatigue, device sprawl, and fragmented portals. Success depends on treating wearable data as part of broader healthcare interoperability solutions.
Prioritizing the Right Use Cases
Not all programs deliver equal value. The most successful health systems start where wearables solve clear problems:
- Chronic disease management: continuous data for diabetes, COPD, and cardiac care.
- Post-discharge monitoring: early detection of deterioration to cut readmissions.
- Pre-op and pre-habilitation: tracking readiness before surgery.
- Behavioral health: sleep and activity monitoring for adherence and engagement.
Each program should link device data to defined clinical goals, target cohorts, and specific EHR destinations.
Standards That Make Data Usable
Device data is only valuable if it flows cleanly into systems clinicians already use. That requires consistency across technical and semantic layers:
- HL7 FHIR for new APIs, with Device and Observation resources.
- LOINC codes for measurements and SNOMED CT for findings.
- RxNorm for medication data, ICD-10-CM for diagnosis alignment.
- SMART on FHIR for secure app launch and consent.
This approach avoids vendor lock-in and ensures data can support care, reporting, and analytics.
Building the Integration Architecture
A reusable blueprint helps scale programs:
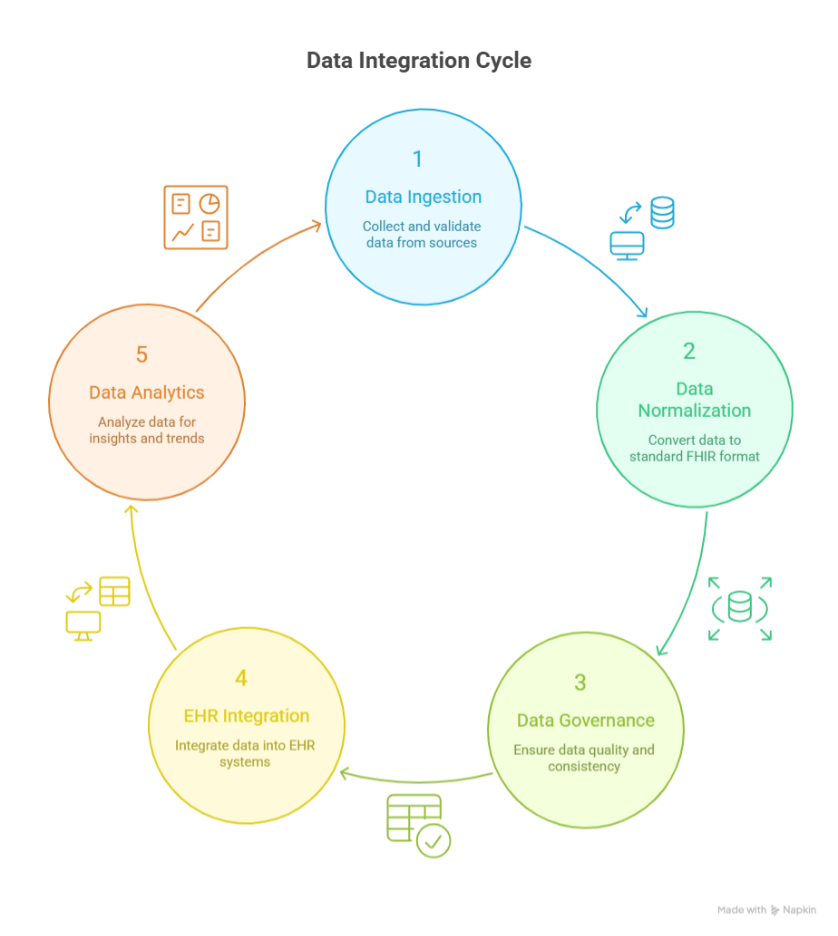
- Ingestion: Device gateways or APIs bring in time-series data. Validate early to prevent malformed payloads.
- Normalization: Convert streams into FHIR Observations with standard codes and provenance.
- Governance: Score data quality, manage terminology updates, and set reproducible transformation rules.
- EHR integration:
- Write-back into vitals or flowsheets for permanent record.
- Sidecar apps for triage dashboards.
- CDS Hooks for in-workflow alerts.
- Analytics: Aggregate by cohort, device, and clinician workload. Track interventions and outcomes.
Workflow Design to Prevent Alert Fatigue
Data without process becomes noise. Effective programs design clear clinical pathways:
- Review cadence: daily for high risk, less frequent for stable cohorts.
- Tiered thresholds: combine baseline deviation with absolute limits.
- Bundled alerts: group episodes of abnormal readings.
- Role-based routing: assign to existing care team work queues.
- Closed loop: automated patient messages or education to reduce manual outreach.
Compliance and Security Guardrails
Wearables often originate in consumer ecosystems. Healthcare integration must close compliance gaps:
- Collect only the minimum necessary data.
- Capture and honor patient consent.
- Ensure vendors provide HIPAA BAAs, security testing, and clear data residency terms.
- Maintain audit trails for data exchange and access.
- Establish playbooks for device loss, outages, or anomalous spikes.
Building the ROI Case
Integration projects need more than clinical enthusiasm. ROI typically comes from four areas:
- Clinical outcomes: better disease control and fewer readmissions.
- Operational efficiency: less manual entry, shorter virtual visits, focused outreach.
- Financial performance: RPM reimbursement codes, fewer denials, optimized staffing.
- Strategic value: stronger patient engagement and data liquidity for research.
Crawl-Walk-Run Rollout
Scaling works best incrementally:
- Crawl: Start with one program and a single integration pattern. Test thresholds, triage, and documentation.
- Walk: Expand to a few cohorts using shared services and governance.
- Run: Offer RPM as an enterprise platform, add payer connections, and formalize ownership.
Common Pitfalls to Avoid
- Device sprawl without standard approval processes.
- Vendor lock-in where raw data isn’t portable.
- Terminology drift as codes and units evolve.
- Shadow workflows in vendor portals.
- Over-alerting from static thresholds.
Governance, standardization, and feedback loops are the antidotes.
Measuring What Matters
Key performance indicators show whether integration is working:
- Patient enrollment and data submission rates.
- Review time per clinician per 100 patients.
- Alert resolution and escalation rates.
- Intervention-to-outcome ratios for target conditions.
- Documentation completeness in the EHR.
Conclusion
Wearables and remote monitoring can transform care delivery — but only when their data is standardized, governed, and embedded directly into clinician workflows. Success lies in a structured rollout, reusable FHIR-based architecture, and careful alignment with privacy and compliance frameworks.
When executed well, wearable data integration is not a side project. It is part of the larger effort to deliver healthcare interoperability solutions that makes information clinically meaningful and operationally sustainable.
FAQs
What standards are best for wearables data to EHR?
Use HL7 FHIR resources such as Device and Observation, with LOINC for measurements and SNOMED CT for clinical findings. Keep identity, consent, and provenance in the payload.
How do teams validate accuracy from consumer devices?
Combine device certification checks, calibration routines, and signal quality tests. Set program-specific acceptance rules before write-back. Flag suspect values for review rather than auto-posting.
What are the privacy risks with remote monitoring data?
Data may originate from consumer apps, which raises consent and scope concerns. Use minimum necessary access, clear consent flows, secure API authentication, and comprehensive audit logs.
How do we integrate without creating another portal?
Favor write-back to native flowsheets or a SMART on FHIR sidecar embedded in the EHR. Use CDS Hooks for in-workflow nudges so clinicians do not switch systems.
Can wearable data feed clinical decision support and AI?
Yes, once normalized and coded. Start with rule-based CDS on top of high-quality Observations. When data quality stabilizes, layer predictive models with governance and monitoring.